What You Have to Know About PCOS
As I work with my clients, I like to identify the root cause of their issues and always start by asking this question: “WHY is this woman’s body doing this?” This could be any woman with PCOS; no two women are alike, so we want to figure out exactly what’s fueling their hormones to be out of balance.
-Dr. Dana Cohen

Understanding PCOS: A Comprehensive Overview of Causes, Symptoms, and Treatment Options for Women’s Health
PCOS is one of the most common yet least understood endocrine conditions that can affect women of childbearing age. I have observed it throughout my career as an integrative medicine physician. It is so common, yet also misunderstood and underdiagnosed. In this article, I provide a comprehensive overview of PCOS. I’ll share the basics of what PCOS is and what it isn’t. Who gets PCOS and how it can impact so many areas of health. We’ll also examine the symptoms and treatment from both conventional and integrative medicine perspectives.
What is PCOS?
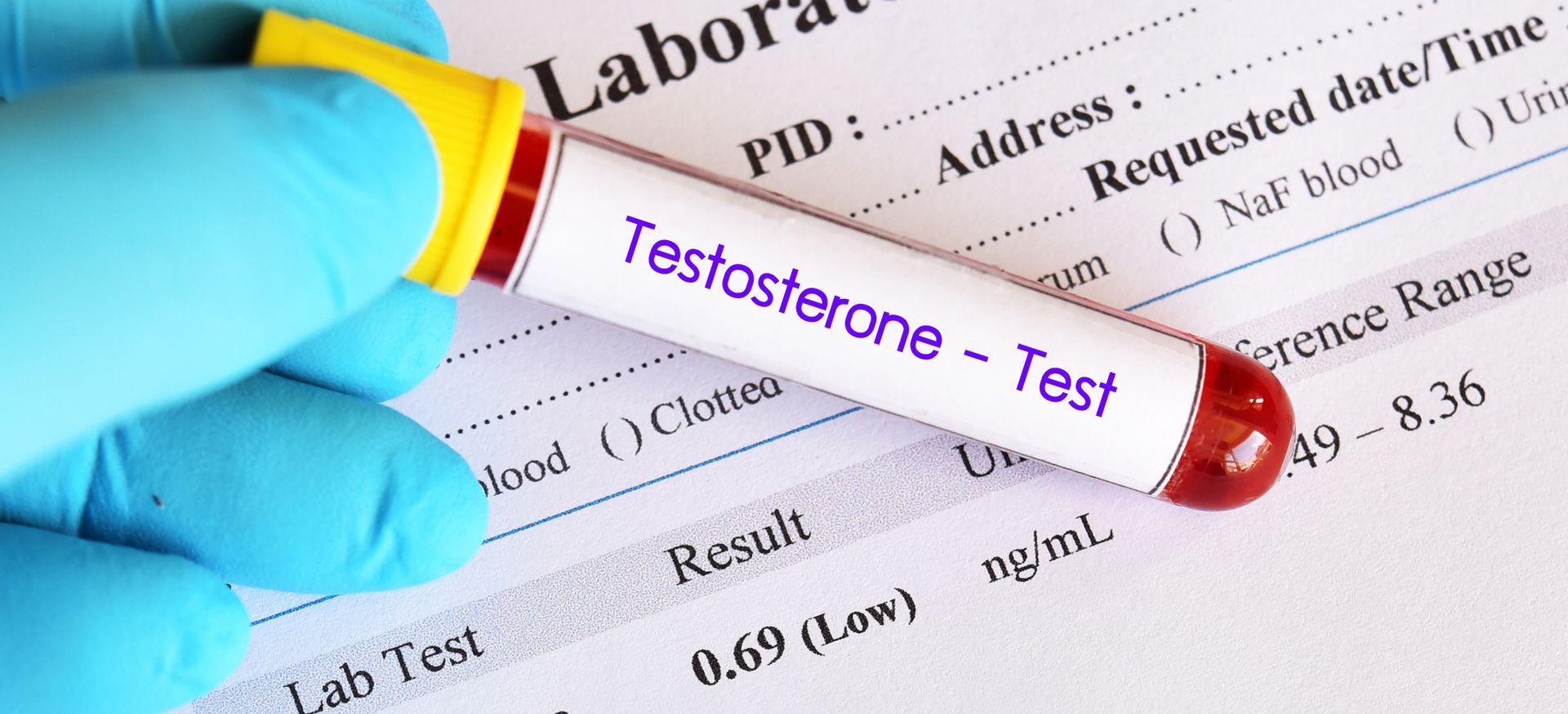
PCOS, at its most fundamental level, is a disease of hormonal imbalance. It gets its name from the fact that women with PCOS may develop small fluid-filled sacs (cysts) on their ovaries. However, not all women with PCOS have these cysts, and, again, what is going on under the hood is a web of hormonal irregularities. Hormonal imbalances involving insulin and androgens (male hormones, like testosterone) are the primary culprits in PCOS. These imbalances can lead to irregular or absent ovulation, causing missed periods and possible fertility issues. However, the effects of PCOS are far-reaching.
The hormonal chaos associated with PCOS can lead to metabolic dysfunction. Weight gain and trouble losing weight are common in women with PCOS, and the risk of insulin resistance and type 2 diabetes is increased. Excess hair growth in typically male pattern areas (Hirsutism), acne, and male-pattern hair loss are common in women with PCOS as well, due to the elevated androgen levels. The mental health impact is also significant, with higher rates of anxiety, depression, and low self-image reported in women with PCOS compared to women without the condition.
The effects of PCOS are felt across the board in women’s health. Short-term effects of PCOS can include painful or missed periods, acne, and excess hair growth, and difficulty maintaining a healthy weight. Due to chronic inflammation associated with PCOS, it can also cause more general symptoms of fatigue, joint pain, and headaches.
Long term, PCOS can be detrimental to women’s health and increase the risk of metabolic syndrome, type 2 diabetes, cardiovascular disease, and endometrial cancer. The risk of gestational diabetes is also higher for women with PCOS when pregnant. One of the most emotionally distressing effects of PCOS is its effect on fertility. PCOS is one of the leading causes of infertility in women. Infertility is associated with significant psychological stress, even in cases where pregnancy is still possible with medical intervention and specialty care. The many aspects of the stress from infertility, on top of the physical burden of PCOS, can be overwhelming for many women. In my experience as an integrative physician, the effects of PCOS on the body and mind cannot be ignored.
PCOS Symptoms
The symptoms of PCOS can vary widely between individuals, and this is one reason why the condition can be challenging to diagnose and may be delayed. The classic triad of symptoms of PCOS, first described in 1990, is:
- Irregular or missed periods
- Clinical and/or biochemical signs of excess androgens (acne, excess facial and body hair growth (hirsutism), and thinning scalp hair)
- Polycystic ovaries on ultrasound.
It is unusual for all three of these features to be present, and one or two are commonly used to define PCOS. As many as one-third of women with PCOS have regular menstrual cycles, and the major feature is androgen excess. A significant number of women with PCOS have polycystic ovaries but few other symptoms, while some women with PCOS have regular cycles and normal ovaries. Although weight gain, especially with a tendency to gain weight around the abdomen, is typical, 20% of women with PCOS are of normal weight. Other symptoms that can be present include skin tags, darkened skin (acanthosis nigricans), sleep apnea, and chronic fatigue. Women with PCOS have a significantly higher prevalence of mood disorders such as anxiety and depression.
PCOS Causes
The underlying cause of PCOS is unknown, but researchers think that PCOS is the result of multiple genetic and environmental factors. PCOS appears to have a strong genetic component, and having a mother or sister with PCOS increases one’s own risk. At the same time, the genetic component of PCOS is incomplete, as the environment in which the affected woman lives is also essential.
Several environmental factors have been identified as affecting women with PCOS, such as chronic stress, exposure to environmental toxins, diet quality, and physical inactivity, which contribute to the development and progression of PCOS. Insulin resistance is also seen in PCOS and occurs in up to 70% of women with PCOS, independent of weight status. In some women, it is thought to be both a cause and a consequence of PCOS. The relationship between insulin resistance and PCOS forms a cycle, as insulin resistance contributes to the development of PCOS, which results in a higher production of androgens, which in turn exacerbate the symptoms of PCOS, ultimately contributing to further insulin resistance.
Traditional Care for PCOS
In conventional healthcare, the first-line treatment for PCOS is pharmaceutical and symptomatic. Birth control pills are commonly prescribed to regulate the menstrual cycle and lower androgen levels. Drugs to improve insulin sensitivity are recommended in the presence of insulin resistance. Clomiphene citrate or letrozole is used to induce ovulation for women who wish to become pregnant.
These medications are effective at treating the symptoms that bring many women to seek medical care, but they do not treat the hormonal and metabolic root cause of PCOS. In addition, many of these medications have side effects that some people find difficult to tolerate. Oral contraceptives may cause nutrient depletion and mood changes. Metformin, a drug used to lower insulin levels, is known for causing digestive issues. If fertility is a goal, interventions may be escalated to include surgical procedures like ovarian drilling or assisted reproductive technologies. While these may be effective for helping to manage the reproductive aspects of PCOS, they do not typically address the full body health consequences of PCOS or guide how to address or manage the condition beyond symptom management.
Functional and Integrative PCOS Treatment
As I work with my clients, I like to identify the root cause of their issues and always start by asking this question: “WHY is this woman’s body doing this?” This could be any woman with PCOS; no two women are alike, so we want to figure out exactly what’s fueling their hormones to be out of balance. My PCOS treatment approach to this is first to get an excellent idea of what the main reasons might be by doing some targeted testing outside of the usual tests that a typical doctor will do and my testing protocol will look like this: extensive hormone testing, metabolic and inflammatory markers and sometimes genetic testing depending on the situation.
Nutrition is key in any integrative approach to PCOS, and while there isn’t a specific “PCOS diet,” most individuals will benefit from an anti-inflammatory food plan that helps keep blood sugar levels stable, optimizes gut health, and provides the body with the proper nutrients it needs to balance hormones. This plan will look different for everyone, but should typically include a high intake of non-starchy vegetables, quality protein, healthy fats, and limited refined carbohydrates.
Supplementation should be individualized and based on specific deficiencies and symptoms; however, certain supplements can be especially beneficial in the treatment of PCOS. For instance, inositol is helpful for addressing insulin resistance and promoting ovulation, while N-acetylcysteine aids in reducing inflammation and supporting antioxidant status.
Lifestyle factors are also a significant part of my approach, ensuring that these women get optimal sleep, practice stress-reduction techniques, and incorporate appropriate exercise, all of which can have a substantial impact on reducing inflammation and supporting hormone balance. Most importantly, the integrative approach gives these women the power and knowledge to help them understand why they are experiencing the symptoms they are and what they can do to overcome them, rather than just learning how to manage the symptoms of the disease.